"How the University of Utah Prepares Family Medicine Residents to Lead Value Improvement Efforts"
NEJM Catalyst Case Study
Susan Pohl, MD, FAAFP, Sonja Van Hala, MD, MPH, FAAFP, Mari Ransco, MA & Jennifer Leiser, MD
Training "In Demand" doctors
[Bob Pendleton:] I’m delighted today to be with one of my favorite doctors, Dr. Susan Pohl. We’re discussing Dr. Pohl’s leadership in value. First, what drew you into the field of medicine?
[Susan:] I studied science in high school and was fascinated how things work. I was drawn to chemistry and physics. I was interested in medicine, but the guidance counselor said, ‘you probably won’t get into medical school, you should think about engineering.’ So I did quite a bit in engineering, and studied engineering in college. I loved the problem-solving, I loved creating new things, it was very exciting. But the speed of change was fairly slow, and couldn’t impact people as much as I wanted. I was drawn back to medicine, applied, and went to medical school. In medicine, I’m able to problem-solve with people, I like the pace and I like being around people. Family medicine is the best of both worlds. It’s the art and science in medicine.
(Quick Clip: 1 minute 45 seconds)
(Full interview: 21 minute 35 seconds)
[Bob:] You have been a pioneer in thinking to equip our trainees with new skills, quality improvement, process improvement-type skills needed to provide value-based healthcare. You’ve integrated that into a training program. What drew you to that? Were you volun-told or did you come naturally?
[Susan:] Early in my career, I was in a regional medical center. We were just starting to look at some of our metrics, and they needed someone to tackle the way we provided care. I went to some quality improvement conferences about how to analyze and improve care. Making processes better just lit a fire within me. It’s safer for physicians and providers. I was excited about improving systems to provide good care every single time we touch a patient.
[Bob:] You’ve taken that spark and interest (and threads from before medical school that I wasn’t aware of), to equip the family medicine residents with the skills to build better systems, and better processes. How did that start? What does your program look like today?
[Susan:] Initially, residents tackled individual projects on their own. They were given the task to learn quality improvement through a few lectures. Then they had to create a team, look at data, and improve the care in their particular practice. Those were very interesting and I think the concepts were taught but it wasn’t team-based.
Several years ago, we decided to integrate resident experience with quality improvement into our day to day operations. So at the Madsen and Sugarhouse clinics, which are the family medicine residency sites, we take time each month to have multi-disciplinary team meetings– MAs, pharmacists, front office staff, RNs, residents, and faculty. Everyone gets together to work on process. We analyze our data. Teams monitor the data over time and are tasked to improve process, so that the outcomes are meaningful and improving. Every resident joins a team when they first start residency. The very first month, they join a team looking to improve. Their second year, they get more exposure and responsibility within the team. Their third year of residency, they lead the team under the supervision of a faculty advisor.
[Bob:] Hearing you describe your program makes me realize that there is no easy button and no short cuts. You identify needing team leadership skills, the ability to analyze data and time with the team to figure how to improve. So that is hard. It requires dedicated time and commitment. What has been the hardest part of actualizing that vision?
[Susan:] Initially, to get the residents really excited, we let them work on anything that they wanted. The residents were excited about the work they were doing, but there were challenges to get data and team buy-in for their projects. As the year went on, they realized that making change is very hard. Excitement waned. They had difficulty completing the work, and difficulty leading their teams.
Several years ago, we decided to shift the work of our teams, to align with clinical metrics like disease management, immunization, disease prevention, screening tests. We have the data, we have buy-in from leadership that these are important metrics. Everyone is on board. The flip side is that residents are initially less excited about these projects. However, their interest grows as they are able to get data, they are able to get buy-in. They learn the importance of alignment in quality improvement, to focus on what’s important for the institution, and what’s important for your entire team.
[Bob:] I’m struck by that description because we are currently in a period of time that’s very externally influenced. We have new provider payment reform called the MACRA legislation or Quality Payment Program by Medicare. The performance period starts in January 2017, right around the corner. In this period, really trying to focus on getting intrinsic value out of the process problem-solving itself–I think that is an important path. Have you seen a shift from them getting intrinsic motivation by being able to move a number? Have you seen that foster intrinsic motivation or are we still not there yet?
 [Susan:] Every resident is different. But early success has helped. For example, improving immunization rates. We used data to break down some barriers and we really moved the dial on immunizations. Leaders produced scholarly work, posters, presented nationally and one practice got an award.
[Susan:] Every resident is different. But early success has helped. For example, improving immunization rates. We used data to break down some barriers and we really moved the dial on immunizations. Leaders produced scholarly work, posters, presented nationally and one practice got an award.
Now the residents see these as professional skills. Just like when you are running a hospital service, you may not be interested in a GI bleed today, but if you have 4 cases of GI bleed, that’s what you’re taking care of because your team needs to take care of GI bleeding; it’s a professional skill. You need to learn the skill because that’s what is coming through your door. What I tell residents now is, “We need you to help improve this measure, and you’re going to learn some skills. These are professional skills. You’ll be able to take this to any project.”
Last year, we tasked a resident to look at STD screening. He did a great job and moved the pendulum. What he was really, passionately interested in is caring for patients using chronic narcotics. He took his skills from his required assignment to use in a much more complex area. But he was passionate about it, he received awards for his work in that area.
[Bob:] It’s one of the reasons I wanted to talk with you. I’m a believer that tomorrow’s physicians will require these new skills. Have you had similar feedback from residents that have gone out into practice? Do they feel better equipped to meet the challenges of our healthcare landscape?
[Susan:] Definitely. As our third year residents interview, they explain that they’ve led teams, have looked at populations and population management, and the value of care delivered. They are sought out by large health systems. One resident told us, “I wanted to talk about this other stuff, but man, all they wanted to talk about during the interview was my experience leading this team.” This becomes a trigger and a motivator for residents. Experience in this area opens doors. It opens doors because you can fill a need. You can fill a need in Salt Lake City, you can fill a need in St. George, you can fill a need in Oregon or California. You can take skills you’ve learned here anywhere because everyone is looking for this skill.
[Bob:] It’s a testament to your leadership, how you’ve visualized and implemented your program. One question I have is this notion of being able to build this competency in your faculty while you are training your residents. How do faculty mentors build their skills in their role so they are learning and getting better at coaching the quality improvement? Talk to me a little bit how you’ve supported your fellow faculty members to row in the same direction?
[Susan:] That has been a challenge. We are learning at the same time. We focus on skills using short lectures to move a project forward and analyze data. As we’re teach residents we also teach the faculty. Our groups look at processes, at the value of the care we provide, include all the faculty, the residents and our staff. They have seen a process go through an entire cycle and maybe an entire year to “see while doing.”
This year, I implemented the value summary. That has been a good way to get everyone on board because as you that to look at your projects, you’re actually dividing the work in bite-sized pieces so that the team knows—okay, we’re going to work on this section. If they need some more information, they can go ask for more information on this one section, and then they can go to the next section. That has helped bring everyone up to speed and has helped create a culture that we all work on this. It’s not just a resident project, it’s a team project.
[Bob:] I’m smiling because when I interviewed Dr. Brigitte Smith earlier, I came to this pessimistic or realistic conclusion that getting doctors where they need to be to lead with the right skills is generation away. Hearing you makes me optimistic. Maybe we’re a half generation away because of the types of things you’re leading.
What do you wish you knew when you starting your residency program?
[Susan:] When we first started, we were inventing our own wheel. We worked in a silo by ourselves trying to create new things and trying to learn by doing. As we matured, we focus on aligning resources all the time, getting as much done with the fewest resources while making sure that you’re meeting nursing, MA, resident and faculty needs, while getting as much done as early as possible. Engaging faculty in other departments is key. Seeing what they’re doing so that you’re not working by yourself.
[Bob:] The work that you’ve done and the lessons you’ve learned, and sharing those lessons with others is a key accelerant for us. I want to thank you for what you do every day. We’re a better place because of people like you.
Podcast originally appeared on Accelerate December 6, 2016. (Recording date: November 22, 2016)
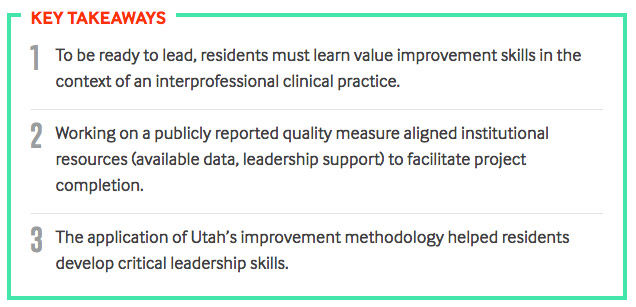
Key takeaways and block quote from NEJM Catalyst publication: "How the University of Utah Prepares Family Medicine Residents to Lead Value Improvement Efforts" published online March 13, 2018.
Susan Pohl
At academic medical centers like the University of Utah, clinicians are expected to teach — but aren’t necessarily taught how to teach. Karen Gunning and Joanne Rolls come from divergent backgrounds — Gunning is a lifelong pharmacist, Rolls a physician assistant — but both are passionate about the principles of instructional design. Turns out, it’s the power of story that supports comprehension for both students and patients.
The practice of medicine is recognized as a high-risk, error-prone environment. Anesthesiologist Candice Morrissey and internist and hospitalist Peter Yarbrough help us understand the importance of building a supportive, no-blame culture of safety.
Vascular surgeon Brigitte Smith is about to start her second year leading a value improvement curriculum for surgery residents. She believes you can’t be a great provider until you’re ready to lead a team to improve care delivery. Here, Smith shares the importance of recognition in motivating residents (and their teams) to learn to improve.
