The Challenge
The Value Equation of Sepsis
Sepsis is a life-threatening infection that can kill within 48 hours. Severe sepsis is the leading cause of death at University of Utah. It accounts for 42% of Utah’s mortality. Sepsis is challenging to diagnose because its early symptoms are similar to other diagnoses. Early diagnosis and rapid treatment are key to survival.
Improving Utah’s care of sepsis patients has a strong value equation. Utah’s value equation is Value = Quality + Service/Cost. Introducing, implementing and spreading standard care guidelines could save 50 lives a year and reduce costs by decreasing length of stay. While the value proposition was straightforward, the team still struggled through stops and starts and years of work.
are redesign focused on a specific condition is often localized on specialty units. But what if the condition touches everyone in the system? Sepsis is a life-threatening, rapidly developing condition that can occur on any service or in any unit. Redesigning the system’s care of sepsis patients meant changing the practice of physicians, nurses, pharmacists, and nurse aids with the support of IT and administrators.
Setting the Stage
The Duo
A partnership between two physicians is the foundation of this improvement effort. Devin Horton and Kencee Graves started as hospitalists at the University of Utah a year apart, after completing their training at Utah. Horton describes Graves as “smart, a hard worker, totally organized,” while Graves praises Horton for his “creativity and vision.” Horton and Graves sat in adjacent offices and frequently shared the travails of their first year as attending physicians.
Both were completely new to value improvement, when they decided to work on sepsis. Horton remembered “I would be frustrated to see patients on consult service who had been decompensating for days…I thought there has to be a better way to do this.” Horton heard a talk by Dr. R. Phillip Dellinger, a renowned sepsis expert. Dellinger’s research and campaign indicated that recognition of sepsis and quickly administered therapy could save lives. “I learned that sepsis is the #1 killer of hospitalized patients. It all came together for me, and I thought ‘holy cow, I can’t believe no one is working on this.’”
One afternoon, Horton wandered into Graves’ office while she was busily planning her first curriculum for a residency quality improvement program. “Want to work on sepsis?” Horton asked Graves. Graves said "Sure. What better way was there to learn quality improvement than to do it?”
Finding the right resources to start
First, Horton and Graves needed to define the problem. They knew the individual patient stories, but they needed data. How long did it take to request the right labs? How long for the labs results to return? How long to begin the correct medication? This was bigger than chart reviews. They needed BIG data, which meant finding a data steward.
After asking colleagues, they met John Arego, a quality data manager. Horton remembered “John Arego was the key that opened up the hospital to us. Arego introduced us to groups we didn’t even know existed.” Horton and Graves were connected to a network of support – quality consultants, value engineers, data managers. This assistance proved invaluable. Arego, quality consultants Tim Nelson and Russell Leslie, value engineers Collin Seabourne and Matt Sanford had the knowledge and social capital to guide a large project. They knew who to ask for information and how to motivate and lead the various subcultures of the hospital. They joined Horton and Graves on the leadership team.
Baseline analysis reveals the need for more team members
Sepsis Education Survey Data
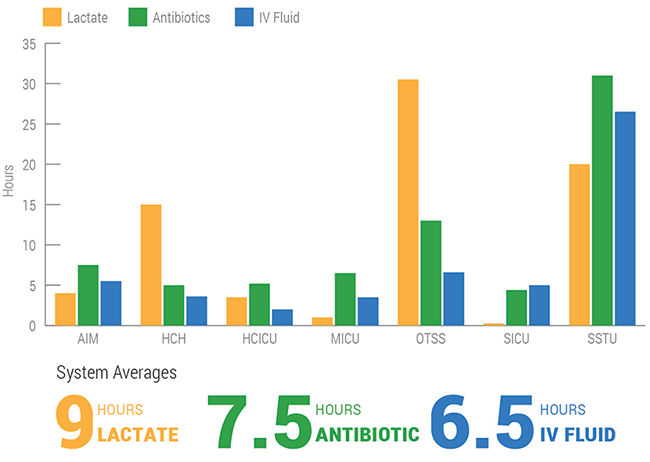
 The sepsis treatment data revealed variation in practice across and within units. Some services and units were better than others at getting the right labs and treatment. But all units were outside of the recommended practice guidelines. Furthermore, the team also realized that physicians, nurses and nursing aids were unable to consistently recognize the tell-tale symptoms of sepsis. Based on the data, the team had two goals: standardize sepsis treatment and help clinicians recognize sepsis.
The sepsis treatment data revealed variation in practice across and within units. Some services and units were better than others at getting the right labs and treatment. But all units were outside of the recommended practice guidelines. Furthermore, the team also realized that physicians, nurses and nursing aids were unable to consistently recognize the tell-tale symptoms of sepsis. Based on the data, the team had two goals: standardize sepsis treatment and help clinicians recognize sepsis.
Lessons learned: Going on the road to change practice
1. Gaining support from key individuals (independently or in small groups) ahead of a large group meeting and bring data driven analysis.
2. Propose flexible criteria with inflexible implementation.
3. Design methods of ongoing engagement.
4. REPEAT steps 1-3 p.r.n.
Download Process Map: PDF
Going on the road: Changing practice
The solution recommended by sepsis experts was an early warning system that dictated awareness of thresholds in specific vitals, followed by specific labs and then antibiotics delivered to the patient within an hour. The team designed a modified early warning system (mEWS) that would fire an alert in Epic, the electronic medical record. Epic scans all inpatient vitals and then calculates a mEWs scoreAHRQ: The Modified Early Warning System (MEWS) is a tool for nurses to help monitor their patients and improve how quickly a patient experiencing a sudden decline receives clinical care. The color-banded patient chart gives a visual cue as to when to calculate a MEWS score. (1-12). A score of 5 or above triggers a cascade of actions. Using an alert is an example of a forcing function, which is a mechanism built into the workflow to prevent specific errors or reduce their impact.
The team decided to pilot their protocol on the Acute Internal Medicine A unit (AIM-A). The team expanded to include front-line nurses, pharmacists and IT. Nurses Sunnie Hadley and Andrew Davies, Jenesy Starkey and Mikayla Davis joined the team. Pharmacist Russell Benefield and Infectious Disease physician Emily Spivak brought their expertise. IT project managers Dean Taylor and Dave Roach began working on Epic.
The team realized they would have to influence dozens of teams who were protective of their independence. Response treatment and expediency varied widely around the hospital. In order to standardize, Horton and Graves would need to convince them that the current care was not working and they needed to adopt a solution.
Tools to change the practice of others
1. Gain support from key individuals (independently or in small groups) ahead of a large group meeting and bring data driven analysis.
Horton was acutely aware of how ideas could get heavily criticized in the large group meeting, so he wanted to take a different approach. Before attending a large meeting, Horton and Graves brought the data and the proposed protocol to individual physicians. He remembered,
Horton and Graves continued to take this approach with other physicians, nurses and pharmacists. They would meet individually or in small groups and present the data comparing current process to the proposed solution. Graves developed detailed analysis, and then Horton or Graves would meet with the services, working their way through the hospital.
Horton reflected on how other physicians responded to their request to change practice.
2. Propose flexible criteria with inflexible implementation
While the best practices model defined specific criteria of suspected sepsis, Horton and Graves used it as a starting place for conversation. Once a physician was ready to talk about solutions, Horton and Graves would ask for their opinion on the mEWS alert criteria and then incorporate their feedback.
Horton remembered how this worked with the hospitalists.
For physicians who were concerned that the mEWS alert would falsely identify too many patients, Horton and Graves suggested a temporary, non-intrusive trial. They temporarily added a mEWS column into Epic without implementing the protocol. Physicians could watch passively and see first-hand if the alert system returned false positives.
Horton remembered talking with a surgeon about the new protocol. The surgeon expressed frustration at the thought of instructing trainees to order more blood cultures and more chest x-rays, after spending a decade coaching them to order fewer. Now, the protocol was suggesting that more tests would have to be ordered for patients who possibly didn’t need it. Horton suggested adding the mEWS column so that the surgeon could see that the alert would identify few false positives.
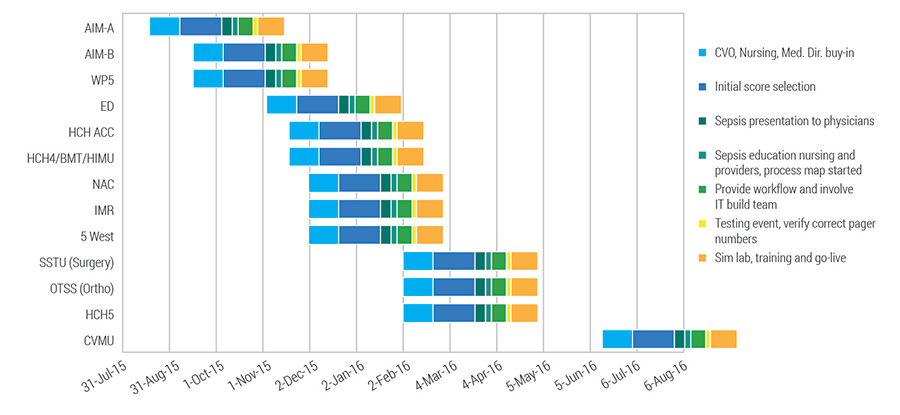
When the physician leader agreed to adopt the protocol, the team worked with the nursing unit to implement. Implementation required specific steps that could not be skipped or missed (which the team had learned during their pilot). Each unit needed education, IT workflow, testing events and live training. Before a unit implemented the new protocol, the nurse manager and nurse educator met with Horton, Graves and Matt Sanford, the project’s value engineer. They would figure out the details of each unit’s implementation—education, call list, follow-up when the mEWS alert triggered.
Project timeline for implementation gantt chart
3. Design methods of ongoing engagement (engagement takes a long time)
As units implemented the new protocol, Horton, Graves, and the team established a review structure. Dr. Horton, Dr. Graves, Matt Sanford, and Epic IT support met with the unit’s nursing leadership and nurse educator every other week for six months. Their task was to review every time the mEWS alert fired. They discussed what went well and what didn’t. Importantly, IT could fix problems with Epic immediately, during the meeting. The group would discuss physician engagement, and Horton and Graves would follow-up immediately if they needed to speak with a physician. After six months, the meetings moved to once a month. To date, attendance at these meetings has been 100%.
4. REPEAT steps 1-3 p.r.n.
It will take more meetings than you think.
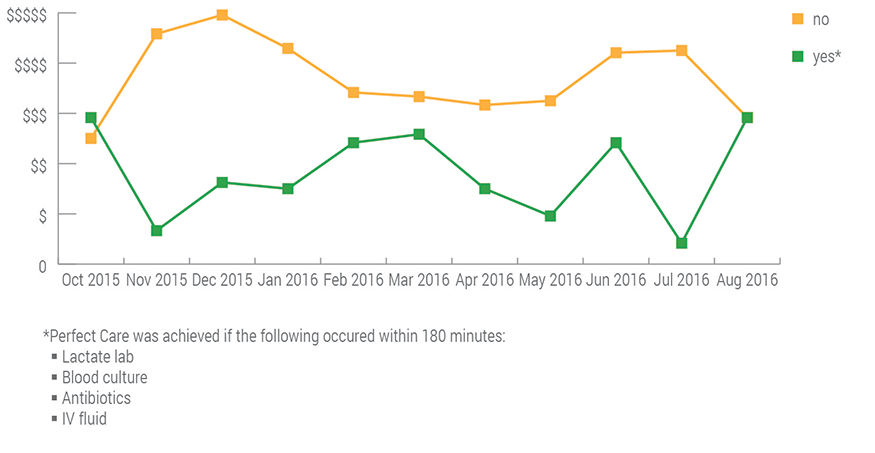
The Metrics
Sepsis (mEWS >5) Mean Cost Per Case and Perfect Care
Reflection
After two years working on sepsis, Horton and Graves have enjoyed success and continued work. Now they have survival cases to talk about when they meet with people. “Being able to show what we had done was really powerful in moving forward,” Graves comments. “We tell them ‘we can do it again.’”
Horton and Graves also value the addition of support from across the hospital. Graves reflects,
Kencee Graves
Devin Horton
Matt Sanford
Chrissy Daniels
Mari Ransco
1 in 3 healthcare dollars is paid for by the United States Health and Human Services, making them the largest payer in the United States. Chrissy Daniels shares this podcast that explains why HHS is changing and how Utah is keeping up.
Your gut tells you a process could be better than it is—how do you back that feeling up with hard data? Senior value engineer Luca Boi shows how undertaking a baseline analysis can jumpstart your improvement project.
Performing a rapid critical appraisal helps evaluate a study for its worth by ensuring validity, meaningful data, and significance to the patient. Contributors Barb Wilson, Mary Jean Austria, and Tallie Casucci share a checklist of questions to complete a rapid critical appraisal efficiently and effectively.
